Tamika Fellows
Rhodes University
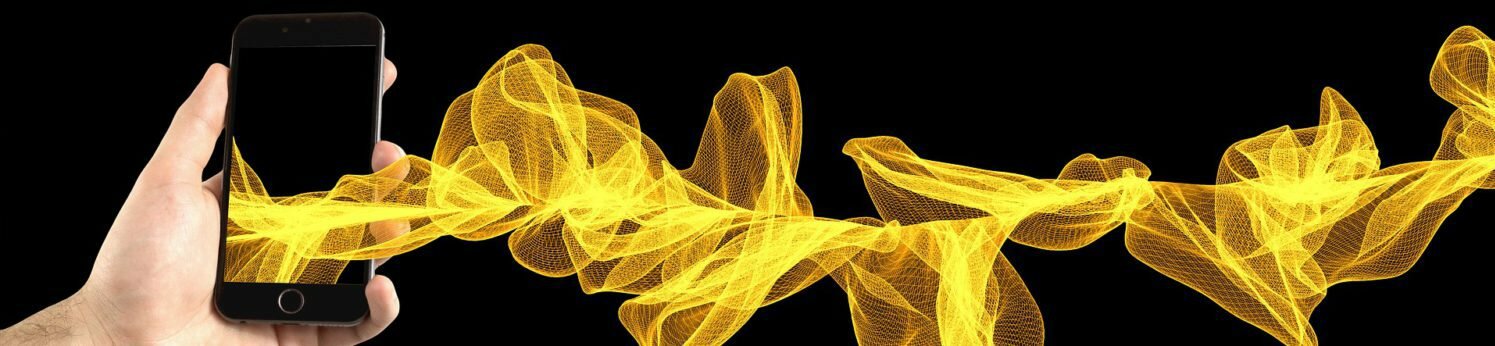
A smartphone retrofitted with an affordable sensor device could give people the power to track their immune status in the comfort of their own homes. This technology, developed by scientists at Rhodes University, could allow HIV-positive individuals to monitor their immune system and know how well they are responding to antiretroviral treatment. This is an important tool in South Africa today where UNAIDS estimates that almost one in five adults is HIV positive.
Currently, HIV-positive individuals usually have to go to a clinic where trained nurses obtain a blood sample. The blood sample is then sent to a centralised laboratory to be analysed using expensive technology. Individuals in urban centres will receive their results in a few days, but for people in rural areas, these results can take up to four weeks. This process, which can be time-consuming, expensive and stressful, means that the average HIV-positive individual in South Africa does not have immediate and affordable access to information about their immune status.
A study presented at the 2012 South African HIV Clinicians Society Conference showed that giving patients the results of their CD4 counts, a marker of their immune health, at the time of their HIV diagnosis could save more than R2.4 billion every year in health care expenditure. A lack of CD4 testing is one of the major barriers constraining the roll-out and scale-up of antiretroviral therapy.
The Rhodes University BioSENS research group, led by Prof Janice Limson and Dr Ronen Fogel, is developing a CD4 test that can be used by healthcare workers and HIV patients to conduct routine CD4 counts, without needing to send samples to centralised laboratories.
CD4 counts are an indication of a person’s immune status and how well their body is able to defend itself against disease. A CD4 count is a measure of the number of CD4 cells, which are helper cells of the immune system embedded with CD4 proteins, present in the bloodstream. These cells form an integral part of the immune system and are responsible for defending the body against disease-causing organisms.
The immune system tries to identify harmful intruder cells and molecules from the millions of other cells in the body. CD4 cells are like tiny sentries that patrol the body: when they find an intruder they set off an alarm that causes the body to send out stronger forces to tackle the intruder. This means that the more CD4 cells a body has, the more alarms can be triggered and the higher the chance of it recognising and finding intruding cells. A healthy body has between 500 and 1600 CD4 cells per cubic millimetre of blood, which is a drop smaller than a pinhead.
CD4 cells are important indicators of health in HIV-positive patients. But the crafty virus specifically attacks these CD4 cells, leaving the body unable to detect and defend itself against other diseases, such as TB.
The HIV virus uses the CD4 protein on the outside of the cell as a door which it tricks the CD4 cell into opening. The virus also “blindfolds” the cell and prevents it from detecting any other intruding cells and sounding the body’s alarm system. Once inside the cell, the virus really gets to work: it reprogrammes the CD4 cell into producing millions of copies of HIV, which the cell then packages and transports into the bloodstream where the copies can invade and attack millions of other CD4 cells.
Because the CD4 cells are “blindfolded” by the virus and no longer display the CD4 protein on their membrane, the body sees the CD4 cells as dysfunctional and destroys them. This is how the CD4 cells of the immune system are depleted in HIV-positive patients.
If their CD4 count falls below 200 CD4 cells per pin-head of blood, they have full-blown AIDS (Acquired Immune Deficiency Syndrome), which means that there are not enough CD4 cells in the bloodstream to be able to detect intruders and signal the body’s alarm. A body with full-blown AIDS is similar to a fortress where all the guards are asleep and most of the cameras have been turned off, so that even the least likely of intruders can get in to rob the mansion and probably even live there comfortably without anyone noticing.
Rhodes University’s CD4 sensor allows patients to be more proactive in the management of their own condition. Our CD4 counting technology is based on the use of molecules known as aptamers.
Aptamers are like keys that fit into biological locks. They are short single-stranded DNA molecules that fold into millions of different shapes and sizes. Because of these different shapes and sizes, there is a high chance that an aptamer will fit perfectly into a specific biological lock.
The BioSENS research group developed an aptamer that specifically binds to the CD4 proteins of CD4 cells. Our aptamer, which carries a specifically designed blue signal molecule, can recognise CD4 proteins on the outside of the cell, bind to them and light up blue. This means that if a CD4 cell is there, the aptamers blaze like little blue flares. The more CD4 cells there are, the more aptamers will light up and the brighter the signal will be.
The CD4 aptamer is easily placed on a simple paper strip. When many of CD4 cells accumulate at one end of the paper test strip, the blue colour becomes visible and can be seen with the naked eye.
The intensity of the colour that develops on the paper test strip shows the number of CD4 cells present in the bloodstream. We can capture the intensity of the colour using a smartphone camera, in a special low-cost case, and an Android app. The smartphone needs to be in a special case, which we 3D print, so that the camera can capture the colour of the strip accurately: if it was too far away from the camera, the strip would appear to be a different colour than it actually is and the person’s CD4 count would not be accurate. From this information, a person can tell whether they are responding to treatment. The results are instantaneous and the test can be conducted in a rural clinic or even at home.
Current diagnostic technology makes use of antibodies, which are large proteins produced by the immune system to identify foreign and harmful cells in the body. They are the gold standard for the recognition and identification of molecules in sensor devices. But antibodies are not only expensive to produce, they are also fragile and do not perform well or last very long in hotter South African climates.
This is why the BioSENS laboratory at Rhodes University is spearheading a drive to replace antibodies with aptamers in conventional diagnostic applications. Not only can locally-produced aptamers be specifically tailored to the needs of South Africa, but they could help both researchers and medical care givers reduce their reliance on expensive imported products.
Very interesting and innovative idea. This indeed can be a game changer, especially in helping to reduce mortality among patients presenting with advanced HIV disease in need of further agressive management (based on the CD4 cell count result). Do you know when the protopyte of your device maybe ready for Phase 1 trials?